Issuing medical certificates
General practitioners (GPs), nurse practitioners, and medical specialists can issue medical certificates. A medical certificate is issued if a patient needs to reduce their hours or change the type of work they do because of their injury.
On this page
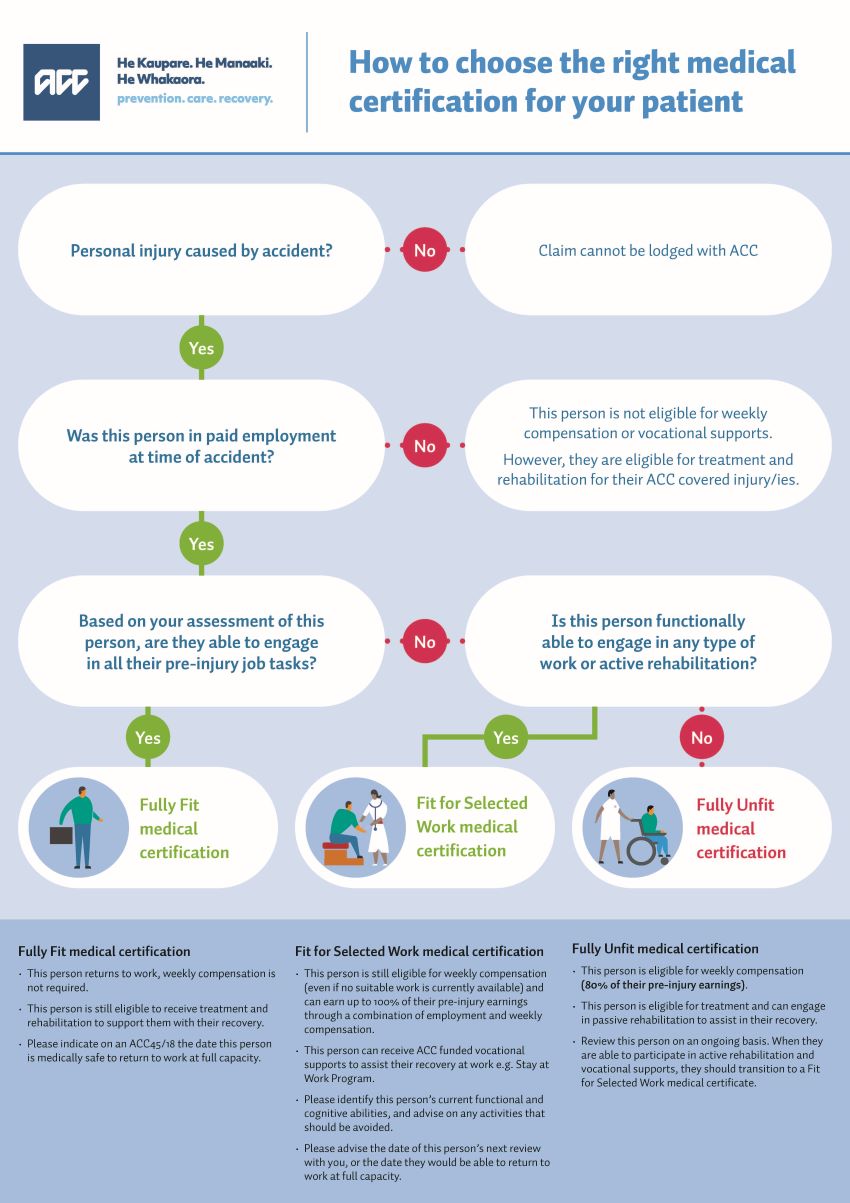
Medical certification supporting guide
Use this print-friendly file to understand how to choose the right medical certification for your patient
Issuing a medical certificate
Issuing the correct medical certificate for your patient’s injury plays an important role in their recovery.
You can certify your patient as either ‘fit for selected work’, ‘fully unfit’ or ‘fully fit’. With the ‘fit for selected work’ and ‘fully unfit’ certifications, your patient will be eligible for weekly compensation from us. This is provided they were earning at the time of their accident.
If your patient was unemployed at the time of the accident, they are not eligible for weekly compensation. But they are still able to receive other ACC support to help them recover from their injury.
How to issue a medical certificate
As a GP or nurse practitioner, you can issue a medical certificate for a maximum of 14 days as part of the initial ACC45 injury claim.
The ACC18 is used to certify beyond the first 14 days.
If your patient is able to engage in active rehabilitation or some work, state on the ACC45 or ACC18 that they're ‘fit for selected work’. Also outline the activities and type of work they can do with their injury.
This also applies to patients who are fully unfit for a few days but are then fit for selected work. You can submit an ACC45 and an ACC18 at the initial consultation to reflect this.
Provide as much detail about your patient’s injury as you can. This helps us work out what support they need.
Submit the medical certificate through your practice management system or our online system.
Medical certificate definitions
This person is able to engage in active rehabilitation or some work with the following support:
- amended duties - changing duties to take account of a condition
- altered hours - changing the times or duration of work
- workplace adaptations - changing aspects of the workplace
- a phased return to work - a gradual increase in work duties or hours.
Scenario
A truck driver has sustained a fractured ankle while working in the forestry industry. While they cannot do certain aspects of their job, for example driving, walking, or lifting, there are other duties they may be able to do. This might be as assisting with administrative tasks if their employer agrees. This person can receive up to 100% of their pre-injury earnings as they recover at work, as we can top up their wages to up.
To be certified as fully unfit, your patient would fit into one or more of the following criteria.
Total inability
This person is admitted to hospital, or confined to bed.
Scenario
A person who has sustained a severe injury, for example, spinal cord injury or traumatic brain injury, and is restricted to bed rest. Or a person who has sustained a traumatic brain injury and requires some time off work in the initial recovery phase to manage fatigue.
Contagion risk or quarantine need
There is a risk of contagion or a need for quarantine as a result of an ACC covered injury, and this person is unable to work remotely.
Scenario
A plumber has undergone external fixation for an open fracture of their proximal humerus. There is an increased risk of infection during initial post-operative recovery phase, and the nature of this person’s job does not allow them to work safely in their usual working environment.
Health and safety risk
Being in the workplace, even with assistance or modifications, poses a specific health and safety hazard to this person, their co-workers, or the general public.
Scenario
A person sustained a severe TBI or requires pain medications as a result of their ACC covered injury. This is having significant impact on the person’s cognitive ability, for example, inability to make sound, safe, timely, and effective decisions. As a result, the person is considered a risk to the public if they drive, or a risk to their co-workers if they cannot respond quickly to high risk work environments.
This person is able to undertake their full pre-injury job duties and hours.
Scenario
An office worker sustained a sprain to their right wrist. They were supported by us, their employer and GP to gradually recover at work and can now complete their full pre-injury duties and hours. While your patient is now considered fully fit for work, they can still receive ACC funded treatment and rehabilitation supports if needed.
Watch: An introduction to medical certification
Hear from Dr Bryan Betty, Chair of GPNZ, as he talks about the fundamentals of medical certification.
Visual
Screen shows An introduction to medical certification. Clock shows watch time of 6 minutes 15 seconds.
Text displays Dr Bryan Betty, Chair GPNZ
Dr Bryan Betty is sitting in a chair facing the camera. A pot plant, water jug, cup of water and pen and notepad sit on a small table beside him.
Transcript
Dr Bryan Betty: Selecting the right medical certification for your patient plays a critical role in their recovery.
If they can still do some of their duties at work while injured, it can actually help them get back on their feet faster.
There's strong evidence that staying connected to work is good for physical and mental wellbeing.
There are three kinds of medical certifications you can provide depending on the person's injury – fit for selected work, fully unfit and fully fit to work.
I'm going to explain the fundamentals of medical certification so you can choose the option that is best for your patient.
Visual
Screen shows Why are medical certificates important? Clock shows watch time of 31 seconds
Screen cuts back to Dr Betty in the chair.
Transcript
A medical certificate documents your assessment of a patient’s capacity to engage in any work and their ability to take part in rehabilitation for their injury.
Issuing the right certification to match a person's injury and circumstances means they can get the appropriate support from ACC to recover, including treatment, rehabilitation, and weekly compensation.
Visual
Screen shows Who needs a medical certificate? Clock shows watch time of 22 seconds.
Screen cuts back to Dr Betty in the chair.
Transcript
Anyone in Aotearoa New Zealand who is employed and is injured in an accident can be eligible for weekly compensation.
The correct type of medical certificate not only determines whether the person needs time off work to recover and financial support from ACC but is also an essential part of your patient’s recovery plan.
Visual
Screen shows Fit for selected work. Clock shows watch time of 1 minute 23 seconds.
Screen cuts back to Dr Betty in the chair.
Transcript
In many situations, your patient will still be able to engage in some work while recovering, although it may mean doing slightly different duties than their normal job. It could be doing fewer hours, lighter tasks, working with modifications or in a different environment.
If you certify a person as fit for selected work, their employer could pay for their productive hours and ACC can top that up with weekly compensation. Being able to perform some tasks may mean your patient can earn up to 100 percent of their pre-injury income rather than 80 percent just on weekly compensation.
But more than that, the international evidence shows that recovering at work is beneficial in other ways. It means the person can keep earning an income and stay connected to their workplace and workmates, who are often a key part of their support networks.
They can keep their skills sharp, or even learn new ones. Getting back to work earlier also means it's more likely they'll remain in employment.
It's important to know that even if their employer has no alternative duties available, your patient will still receive weekly compensation.
Visual
Screen shows What’s an example of someone who’s fit for selected work? Clock shows watch time of 21 seconds.
Screen cuts back to Dr Betty in the chair.
Transcript
Let's say a truck driver suffers a fractured ankle while working in the forestry industry.
There will be parts of their normal job they can't do, like driving, walking or lifting.
But if their employer agrees, they might be able to do other work like helping with administrative tasks.
Visual
Screen shows Fully unfit to work. Clock shows watch time of 37 seconds.
Screen cuts back to Dr Betty in the chair.
Transcript
There will be times where you need to certify a patient as fully unfit to work.
They may: need to be admitted to hospital or are confined to a bed. Need to isolate because of an infection risk as a result of their ACC covered injury and can't work remotely. Or pose a specific health and safety risk to themselves, their co-workers, or the general public.
If your patient was working at the time of their injury, they can receive 80% of their pre-injury earnings while on a Fully Unfit Medical Certificate.
Visual
Screen shows What’s an example of someone who’s fully unfit for work? Clock shows watch time of 23 seconds.
Screen cuts back to Dr Betty in the chair.
Transcript
A person sustained a severe Traumatic Brain Injury or requires pain medications as a result of their ACC covered injury, which is having significant impact on the person’s cognitive ability posing a health and safety risk to themselves or others.
Visual
Screen shows Fully fit for work. Clock shows watch time of 25 seconds.
Screen cuts back to Dr Betty in the chair.
Transcript
The third and final category is fully fit for work.
This means your patient can perform the full range of their pre-injury job.
Even though they will no longer receive weekly compensation, it's still important to complete this so your patient can receive the appropriate ACC-funded support for their recovery.
Visual
Screen shows What’s an example of someone who’s fully fit for work? Clock shows watch time of 19 seconds.
Screen cuts back to Dr Betty in the chair.
Transcript
Someone who's fully fit for work might be an office worker who has a sprained ankle but can still complete all their pre-injury duties and hours.
While they will no longer receive weekly compensation, they are still able to receive ACC funded treatment for their injury.
Visual
Screen shows Teamwork makes recovery work. Clock shows watch time of 31 seconds.
Screen cuts back to Dr Betty in the chair.
Transcript
As your patients’ primary care provider, you have an important role in supporting their recovery.
Completing an assessment of their capacity to work plays a key role in helping your patient to recover at work and return to their everyday activities as soon as possible.
And that's the basics of medical certification.
If you need more information, there is plenty of resources on ACC's website.
Thanks for watching.
Visual
Screen shows For more information and resources visit acc.co.nz/health-providers.
Screen changes again to show the ACC logo and tagline He Kaupare. He Manaaki. He Whakaora. Prevention. Care. Recovery.
Assessing your patient
There are three components that contribute to work capacity — ability, tolerance, and risk. Based on these factors and the assessment you make, the advice you give your patient and their employer can influence how they view their injury as well as their recovery.
Use the ability, tolerance, and risk model to inform the medical certificate.
- Specify what your patient can safely do with their injury — both cognitively and physically.
- Set out your diagnosis, treatment, or rehabilitation recommendations and prognosis, if appropriate.
- Set out any appropriate adjustments to your patient’s work such as hours, travel, tasks, and environment.
- Specify key dates for staged return to work.
- Specify what your patient must not do – to keep them or others safe.
- Outline what may constitute a risk to your patient, for example, certain activities or situations.
- Detail any specific actions that should be taken to reduce risk, for example, changes to work hours or tasks, the environment, equipment or breaks.
When the medical certificate ends
When your patient’s medical certificate ends and they require ongoing certification, you’ll need to issue a new certificate to make sure they continue to receive the support they need.
You can do this by submitting an ACC18 form. The ACC18 form is also used to indicate medical clearance if your patient is now fully fit to work. Your patient can continue to receive treatment and support for their injury if they are cleared as fully fit to work, however their weekly compensation will stop.
Issuing a medical certificate beyond three months
We understand that every person’s injury and recovery journey is unique to them and for some injuries it may be appropriate to issue a medical certificate for a period longer than three months.
Patients with stable serious injuries can get approval for one-year medical certificates. Longer medical certificates (6 to 12 months), for non-serious injuries are considered on an individual case-by-case basis.
When considering longer medical certificates, we need to take a few things into consideration including, but not limited to:
- If functional restrictions have stabilised
- If long term supports are needed
- The person’s health is not fragile or unstable
- The person is engaged with treatment and rehabilitation
- There is an agreed plan in place for regular monitoring. That might be via regular engagement with us or via the wrap around supports that have been put in place.
If you have a patient you think may meet this criteria, the best place to start is a conversation with the ACC team member managing their claim.
Contact us
If you have any questions, contact us:
Phone 0800 222 070 (Monday to Friday, 8am to 6pm)
Email providerhelp@acc.co.nz
